ENDODONTICS AND ESTHETIC DENTISTRY(14)
Any tooth with a questionable pulp should be endodontically treated prior to placing an etched cast restoration. Frequently, this restoration is used to replace an anterior tooth that has been lost as a result of trauma. It is reasonable to assume that the adjacent teeth may have sustained injury as well. Therefore, it is imperative that the pulp and periapical status be ascertained before bonding the restoration in place. However, if faced with root canal therapy, the access cavity must be kept as small as possible. The likelihood of weakening the bond is great. In most cases, a new #2 or #1558 carbide bur and a copious water spray will minimize heat and reduce the vibration, which is the cause of debonding. Occasionally, it is more practical to prepare the access cavity through the labial surface, in particular when dealing with lower incisor teeth that are lingually inclined (Figures 19-50A to D). The distinct advantage of direct access without disturbing the casting is immeasurable. The opening can then be repaired with a light-cured composite resin. Cosmetically, the lip and smile lines should be considered before using this approach. Communicating the benefits of this approach and having the patient accept the technique before proceeding are essential.
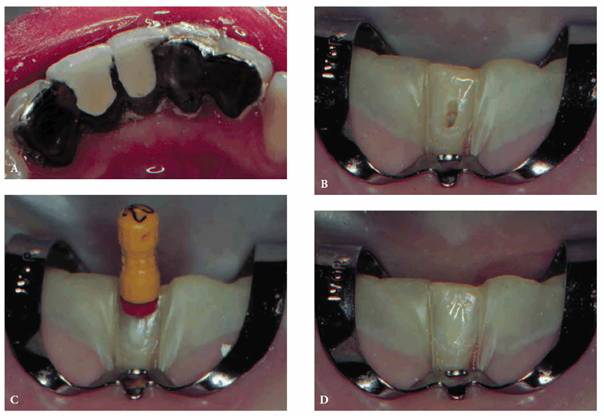
Figure 19-50A to D: Access alternative for an etched cast bridge: (A) five-unit bridge, (B) access cavity prepared on labial surface, (C) measurement file in place, and (D) composite resin repair of access cavity.
Retentive Value After Access Preparation
In addition to esthetic compromises that occur as a result of access preparation, crown retention also becomes questionable. An in vitro study by McMullen et al. showed that the retentive value of a porcelain-fused-to-metal crown was decreased 60.17% following access cavity preparation.19 In a follow-up study, McMullen et al. showed that the retentive value of the crown could be increased 237% over its original value if the crown was recemented with polycarboxylate cement and the access cavity was filled with amalgam.20 However, it is rare that a crown or a bridge is removed after final cementation to allow for endodontic therapy. Unfortunately, retentive value following the filling of the access cavities with amalgam alone has not been studied. With this is mind, filling an access cavity with amalgam after endodontics may not restore it to an acceptable level. This reiterates the need to perform elective endodontics whenever a risk exists prior to the fabrication and cementation of a crown (Figure 19-51).
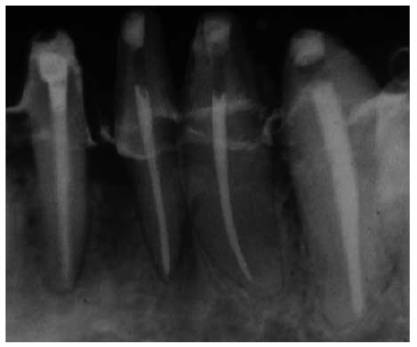
Figure 19-51: Endodontic therapy completed prior to fabrication of final castings on four mandibular anterior teeth with questionable pulpal health.
When faced with unusual situations (eg, occlusal rests and attachment receptacles in removable partial denture abutments), innovation enters the picture. To preserve their usefulness, attempts should be made to keep away from the attachment area. The final access preparation outline should be finished near the attachment but not encroach on it. The shape of the preparation may be decidedly atypical, but the preservation of the mechanical lock integrity will be retained.
Instrumentation/Debridement
The goal of this phase of endodontic therapy is to eliminate all microorganisms from the canal system by completely removing organic and inorganic debris. The objective is to accomplish instrumentation yet maintain the constriction of the canal apex and the flare of the coronal aspect. This canal design will accommodate condensing instruments during the gutta-percha compaction yet confine the filling materials within the canal. Thorough debridement and hemorrhage control will not only ensure endodontic success, they will also prevent discoloration of the crown. This is an extremely important esthetic consideration. Crown discoloration can stem from blood entering the dentinal tubules followed by latent red blood cell degeneration. Severe pulpal bleeding usually occurs when an acutely inflamed pulp is not entirely removed during extirpation. Once an accurate measurement is ascertained, further debridement of the canal and subsequent shaping coupled with copious irrigation with 2.5% sodium hypochlorite (NaOCl) will normally control the hemorrhage. If, on occasion, the flow continues, full-strength 5.25% NaOCl should be used as the irrigant. The solution should remain in the chamber for periods of 5 to 10 minutes.
Today's suggested medication in teeth with vital and necrotic pulps is calcium hydroxide, which does not cause tooth discoloration. However, one still encounters discolored endodontically treated teeth that have been discolored by medication, root canal cements, and paste fillings. Their removal, as well as bleaching procedures, may return the crown to its optimal color, but the duration of the esthetic improvement may be short. Patients should be advised of this fact.
Sealing the Canal System
The final phase of treatment and the key to successful endodontics is the sealing of all portals of exit from the canal system. Here again, esthetic consideration revolves around discoloration of filling materials. A nonstaining root canal cement (ie, Roth 801, Roth International,
The canals should be filled completely as confirmed by radiographs. The excess gutta-percha and root canal cement should be removed 2 to 3 mm apical to the cervical line to prevent discoloration (Figure 19-52). In periodontally involved teeth where longer crowns are planned, the root-filling materials should be removed to the bone level. A 2-mm layer of white temporary stopping should be placed over the gutta-percha.25 Remnants of the cement may be removed with alcohol. A tooth- colored restorative material (ie, composite resin or glass ionomer cement) may be used to fill the rest of the canal and chamber when a post and core are not indicated.
The coronal restoration should be placed as soon as possible after completion of the root canal treatment if it is not placed at the time when the canals are filled. There is now building evidence that the coronal restoration is as important, if not more important, in microbiologically sealing the root canal system as the root canal obturation material (Figures 19-53A and B). In a recent study, Ray and Trope evaluated the radiologic quality of both coronal and canal obturations.24 It was demonstrated that a tooth with good coronal and root seals had the best rate of absence of periapical lesions (91.4%). Good restoration resulted in significantly less incidence of periapical lesions than good endodontic filling (80% versus 75.7%). Poor restoration resulted in significantly more periapical lesions than poor endodontic fillings (48.6% versus 30.2%).
A proper finish of both the temporary and the final filling material is essential so as not to irritate the patient's tongue or soft tissue. Thirty-bladed finishing instruments (ETUF, OS 1, Brasseler) are perfectly suited to provide the smoothest margins for both the material and especially the marginal remnants of the existing restoration. Gold restorations are particularly susceptible to rough edges that need finishing with the 30-bladed instruments.

Figure 19-52: Gutta-percha root filling cut back 3 mm apical to the cervical line to prevent discoloration. Two millimeters of white temporary stopping is placed over the gutta-percha. This space will be restored with composite resin. The adjacent tooth will be restored with a crown.

Figure 19-53A and B: (A) Thirty-five years after root canal therapy. The teeth are asymptomatic, and there are no radiographic changes. (B) Three years after distobuccal root resections and new castings. Periapical lesions developed around the mesiobuccal roots. During the extended treatment phase, the coronal ends of the silvers points were periodically exposed to saliva.
- on 01.11.2012 [endodontics]
- on 01.11.2012 [endodontics]
- on 01.11.2012 [endodontics]
- on 10.13.2011 [endodontics]
- on 12.15.2010 [endodontics]
- on 08.11.2010 [endodontics]
- Long Island College Hospital - [education]
- Faculty of Dental Medicine - H [education]
- The American Association of Or [organize]
- Summer Institute in Clinical D [organize]
- Academy of Osseointegration [organize]
- University of North Carolina a [education]
- American Orthodontic Society [article]
- American Equilibration Society [article]
- Niigata University - Japan [education]
- University of Buffalo [education]