ENDODONTICS AND ESTHETIC DENTISTRY(15)
Bleaching endodontically treated teeth has been a successful part of the endodontic treatment armamentarium. When indicated, the procedure should be instituted at the completion of the root fillings. The results are satisfying, and the patient can readily see the change in tooth appearance.
Unfortunately, a liability associated with bleaching, external root resorption, has appeared in the literature and has been demonstrated in research studies.32 External resorption is the result of an injury to and a subsequent reaction in the periodontal ligament. The use of 30% hydrogen peroxide (Superoxol, Sultan Chemists) and/or heat has been demonstrated to increase the probability of resorption.18 Microscopic opening in the dentinal wall in the cervical region that is not covered by enamel or cementum may allow for the penetration of the bleaching solution to the periodontal ligament. This morphologic abnormality occurred in 5 to 10% of the teeth examined.15 Acid etching of the chamber has been advocated prior to bleaching to allow for deeper penetration of the Superoxol. Heat, Superoxol, and acid etching of the chamber increase the probability of resorption (Figures 19-54A, and 19-54B) and should be avoided, and a kinder, gentler technique should be used.

Figure 19-54A: External cervical resorption 4 years following bleaching with 30% Superoxol (Sultan Chemists) and heat.

Figure 19-54B: Two years after orthodontic extrusion and a surgical approach to repair the resorptive defect.
Walking Bleach Technique
A solid, well-condensed gutta-percha root filling is a prerequisite to bleaching discolored endodontically treated teeth. This should be confirmed with a radiograph. If the root filling is inadequate, it should be redone. Once it has been established that the gutta-percha filling is adequate, it should be removed 2 mm apical to the cervical line, and the reservoir that is created should be filled with a zinc oxide eugenol temporary filling material such as IRM (DENTSPLY/Caulk, Milford, DE). All remnants of root and crown filling should be removed from the chamber. The chamber is washed with 70% alcohol. Sodium perborate powder mixed with water or 3% hydrogen peroxide to a resin-like consistency is packed into the chamber with a plastic instrument. Excess moisture is absorbed with a cotton pellet. The access cavity is closed with a good temporary filling material. An effort is made to ensure a total seal by removing the bleaching agent from the access walls. The maximum bleaching effect takes place within 48 hours (Figures 19-55A, and 19-55B). The tooth is evaluated for improvement after that time. Application of the paste is repeated until an acceptable result is achieved, which is usually two to three applications. A case of severe discoloration could take even more applications. Rivera et al. recommended the placement of a 2-mm layer of white temporary stopping over the gutta-percha root filling following intracoronal bleaching. This is followed by a thin layer of an auto cure glass ionomer cement. The remaining access cavity is then restored with a composite resin. This approach serves two purposes: (1) prevention of microleakage and (2) prevention of iatrogenic perforation if future bleaching or retreatment of the root canal therapy is required by providing different textures of filling materials with slight variations in shading.25

Figure 19-55A: Discolored maxillary canine with a necrotic pulp.

Figure 19-55B: Forty-eight hours after the completion of root canal therapy and placement of a walking bleach.
This walking bleach procedure was introduced by Spasser over 40 years ago.26 The combination of sodium perborate and water apparently produces a sufficient oxygenating effect to bleach internal stains and is believed to be much gentler to the periodontal ligament.14 In vivo and in vitro research studies have confirmed its efficacy. Its obvious advantage lies in its ability to produce the desired result without the liability of root resorption, which is associated with the use of Superoxol and heat.
TRAUMA
The era of the 1980s and 1990s and the new millennium has been one of participation, an era of sports and speed. With it came the concurrent hazard of dental injury. Any blow to a tooth, regardless of its intensity, can cause pulpal damage or pulpal necrosis. The need for endodontic treatment is predicated on the physiologic response of the pulpal tissue and periodontal ligament.32 The esthetic interest in traumatized teeth centers more around the hard tissue damage even though the associated pulpal problems can greatly influence the treatment plan. Crown discolorations, fractured crowns, fractured roots, root displacements, and external resorption are the normal challenges. These problems and their endodontic implications will be discussed individually.
Crown Discolorations
The etiology of tooth discoloration can be congenital, chemical, metabolic, or traumatic. A tooth can absorb a blow without causing a crown or root fracture, yet the force may be sufficient enough to rupture the blood vessels of the pulp. The released blood enters the dentinal tubules, and a reddening of the crown may occur (see Figure 19-2). Treatment of this condition is immediate pulp extirpation followed by complete root canal therapy and bleaching. The sooner that treatment is initiated, the better the prognosis of the bleach. When the tooth is left untreated, the degeneration of the blood cells within the tubules and the necrotic tissue of the chamber will soon cause the crown of the tooth to turn a noticeable gray or black. Treatment is still endodontics; however, bleaching may be more difficult, and color regression after bleaching may occur within a shorter period of time. Often the pulp survives the injury but, unfortunately, undergoes a dystrophic calcification. The density of the tubular reparative dentin and its tendency to totally calcify the coronal pulp chamber cause the tooth to darken to a brownish-yellow hue (see Figure 19-7A). Owing to the obliteration of the chamber and the canal, endodontic treatment of brown-yellow discolored teeth becomes extremely difficult, and bleaching is highly unpredictable.
Crown Fractures
In the fracture of a crown that does not involve the pulp, or a so-called uncomplicated crown fracture, the pulp most often survives without further complications (Figure 19-56). Apparently, when the crown fractures, the force is dissipated and therefore is not transmitted to the root or periodontal ligament. For this reason, the internal tissues remain unharmed. When sufficient tooth structure exists to retain a crown or composite build-up, the exposed dentin is covered with calcium hydroxide and bonded with composite resin until a deferred vitality analysis can be determined at 2, 6, and 12 weeks after the trauma. A true pulpal diagnosis may be determined at this time, and the final restoration may be safely considered.
If the remaining tooth structure is insufficient to adequately retain a restoration, the need for endodontics should be considered. Although an argument may exist to support the use of pin-retained restorations, the degree of injury of pin placement and the risk of fracture predispose elective endodontics and a full crown. The only exception would be a tooth with incomplete root apex formation. Once the root canal therapy is completed, a post and core can be fabricated to provide the ideal restorative condition. However, when the pulp is exposed, endodontic intervention is indicated (Figure 19-57): either complete root canal therapy when the root is fully formed or an apexification procedure in a tooth with an open apex.2 Innovative solutions are required to provide for the esthetic needs of these younger patients (Figures 19-58A to C).

Figure 19-56: Crown fracture with no exposure; the pulp remained vital.
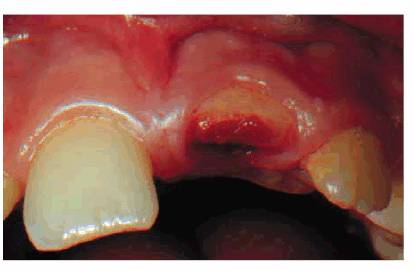
Figure 19-57: Crown fracture exposing the pulp. Root canal therapy was performed.
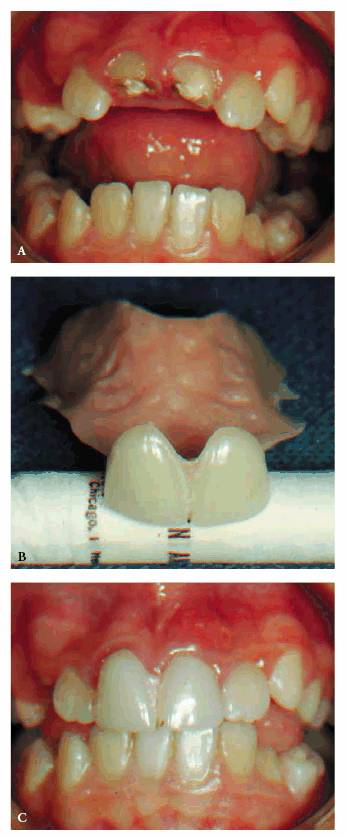
Figure 19-58A to C: Maxillary central incisor teeth: (A) crown fracture and pulp exposures requiring root pulpotomies because of immature apices, (B) a flipper was fabricated for this 9-year-old patient to satisfy the esthetic requirement, and (C) the removable denture in place.
- on 01.11.2012 [endodontics]
- on 01.11.2012 [endodontics]
- on 01.11.2012 [endodontics]
- on 10.13.2011 [endodontics]
- on 12.15.2010 [endodontics]
- on 08.11.2010 [endodontics]
- Long Island College Hospital - [education]
- Faculty of Dental Medicine - H [education]
- The American Association of Or [organize]
- Summer Institute in Clinical D [organize]
- Academy of Osseointegration [organize]
- University of North Carolina a [education]
- American Orthodontic Society [article]
- American Equilibration Society [article]
- Niigata University - Japan [education]
- University of Buffalo [education]