ENDODONTICS AND ESTHETIC DENTISTRY(16)
Root Fractures
Horizontal fractures of the root present unique problems, and the degree of difficulty is relative to the level of the break. It is very possible, and it occurs in a significant number of cases, that separation of the hard structure of a tooth can occur; however, the elasticity of soft tissue thwarts pulpal separation. For this reason, no root canal treatment is indicated and should be considered only when signs or symptoms indicate that an irreversible inflammatory reaction has occurred. When situations arise that warrant attention, the following alternatives are available.
For those fractures involving the apical third of the root, endodontics is performed, if the pulp necroses, to the level of the break, and the separated tip is monitored because most likely the pulpal tissue in it is healthy and does not need any treatment. In the case of a periapical lesion around the apex of the apical portion, surgical extraction is the only treatment possible (Figures 19-59A and B). As to its restorative implications, there is usually sufficient root length that adequate post preparation can be accomplished without reaching the break level and jeopardizing the seal.
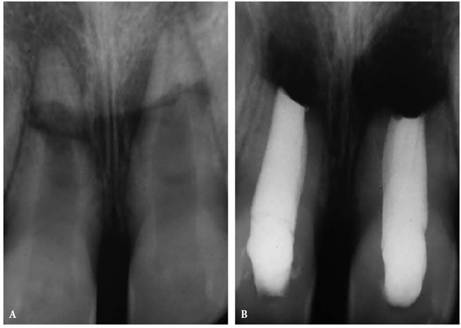
Figure 19-59A and B: Root fracture in the apical third. (A) Maxillary central incisors, horizontal root fractures with pulp necrosis. (B) Root canal therapy in the coronal segments. The apical portions of the roots were surgically removed.
Mid-root breaks create more challenging problems, the first of which is mobility. Owing to the crown:root ratio being reduced to less than one to one, stability is impaired, and a splint must be fabricated (Figures 19-60A to C). These teeth must be monitored periodically to check pulp vitality and periodontal ligament damage. Many of these teeth maintain vital pulps and a healthy periodontium and need no endodontic intervention (Figures 19-60D and E). However, if the pulp becomes necrotic, pulp extirpation is required. Endodontic options are maintaining and filling the coronal segment to the break, instrumenting both segments and uniting the segments with either gutta-percha or the more solid Vitallium (Austenal, Chicago, IL) pin, and removing the apical segment and inserting a Vitallium pin through the coronal segment and extending it to the height of the vacant apical alveolus (Figures 19-61A to C). Such endosseous stabilizers are highly successful as long as there is no communication between the pin and the oral cavity by way of the crown or the periodontium. For this reason, the pin should be reduced to a coronal level within the canal to allow the chamber to be sealed with a bonded resin filling. This obviously presents a problem when a post and core is needed to provide an adequate crown stump. Realizing that post length will be curtailed, the dentist must consider splinted units in the final treatment plan or extraction.
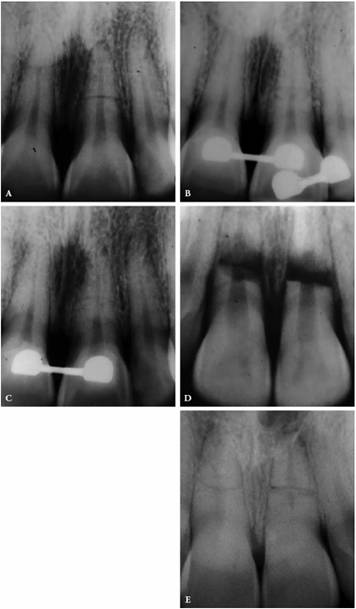
Figure 19-60A to E: Mid-root fractures. (A) Mid-root fracture maxillary central incisor with minimal displacement. (B) Tooth splinted to adjacent teeth. (C) Six years postfracture, there is excellent root healing, and the pulp remained vital. The patient insisted on retaining the bonded bracket-arch bar palatal surface splint. (D) Mid-root fractures of maxillary central incisor teeth with severe displacement. (E) Five-year-check radiograph. The treatment consisted of reducing the fracture and splinting with orthodontic brackets and an arch bar for 16 weeks. Vital pulps are present.
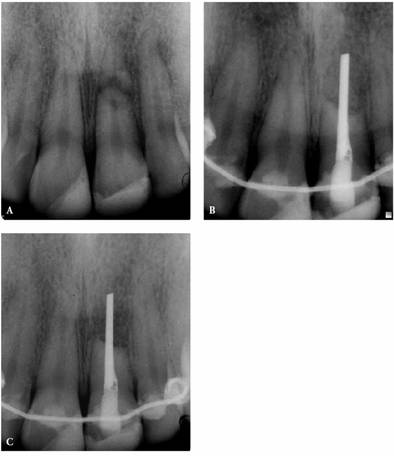
Figure 19-61A to C: (A) Mid-root fracture with pulp necrosis and sinus tract formation. (B) Treatment included pulp extirpation, Vitallium (Austenal) pin implant, bonded splint and bone graft, and guided tissue barrier. (C) Sixteen-month check-up shows deposition of bone in the graft area. Even though the tooth was firm, the patient insisted on retaining the splint.
Root fractures that occur in the coronal third present by far the most difficult situations. The crown:root ratio is adverse, mobility is critical, and the prognosis is grave (Figures 19-62A and B). The coronal segment is too short to retain, and the options for the root segment are extraction followed by a single tooth implant or bridge, vertical extrusion (Figure 19-63), or embedding of the apical segment. The loss of the root would ultimately lead to the loss of the alveolar integrity and the reduction of the alveolar height. Unless ridge augmentation is performed into the vacant alveolus, an unesthetic bridge is inevitable. Endodontically treating the segment and further reducing the root coronally to a level at least 2 mm above/below the crestal height will enable bone to form across the coronal root surface. The embedded root will maintain the alveolar shape, form, and height. A fixed partial denture can then be fabricated without fear of alveolar shrinkage.

Figure 19-62A and B: Root fractures in coronal third of root requiring extraction: (A) maxillary lateral incisor and (B) mandibular lateral incisor.

Figure 19-63: Maxillary lateral incisor with a root fracture in the coronal third. The root is long enough to consider a vertical extrusion.
Perhaps the most favorable treatment would be extrusion of the root segment.11 Endodontics is performed on the submerged root, and a post space is prepared to the normal depth. A stainless steel pin or post, prebent to form a hook that will extend approximately 4 mm into the oral cavity, occlusion permitting, is cemented in place. An arch wire is adapted to the labial surfaces of the two adjacent teeth on either side of the injured tooth. The wire is contoured to bend into the lingual space and create a 180-degree angle with the long axis of the root segment. The labial surfaces of the adjacent teeth are acid etched, and the wire is bonded in place. Ligature bands are wound around the wire and the hook. Owing to the perpendicular angle forces, the root will extrude into its predetermined position. Once the root segment is extruded to a level beyond the crest, it is prepared and impressioned. The active force is eliminated, and the root is held in a passive position for a period of 6 to 10 weeks. This enables the resistant forces of the periodontal fibers to become stable and minimize the possibility of root regression. Occasionally, postextrusion periodontal probing will reveal the need for crown lengthening. Once the dentist is confident of root stability, the final post core and crown can be fabricated with certainty.
Displaced vertical root fractures offer little hope unless the angle of the break terminates at a level that offers the options discussed for a horizontal coronal fracture.
Luxation and Avulsion
The prognosis after severe luxation and avulsion injuries has dramatically improved in the last few years because of a better understanding of how those injuries should be treated. If a tooth is replaced into its original position within a few hours after the injury, or in the case of avulsion replanted within 30 to 60 minutes after proper storage and root canal therapy is initiated 7 to 10 days later, the periodontal ligament will, in most cases, heal without any significant problems.3 Luxated or avulsed teeth that were not properly treated or that suffered a massive injury to the periodontal ligament could present atypical problems created by subsequent ankylosis and root resorption.
Ankylosis without excessive resorption is not a serious problem unless the tooth fuses to bone in a location that creates an esthetic problem. Such is the possibility when the tooth is replanted on a child before the maxilla has had the opportunity to complete its growth. The maxilla continues to develop to adulthood, at which time the injured tooth is superior and labial to the adjacent uninjured incisors. When extracted, ridge augmentation and grafting are required to close the labial mucosa and reconstruct an esthetic alveolar ridge level. Currently, there is no treatment known to arrest ankylosis once it has started. In most cases, root canal treatment will not have any effect on the process because it is caused and maintained by the damage to the periodontal ligament.
Inflammatory root resorption presents a somewhat different situation. The endodontic objectives are centered on the arrest of the inflammatory processes that were initiated by damage to the periodontal ligament, which are being maintained by irritation from an infected root canal system and dentinal tubules. Presently, treatment consists of periodic applications of calcium hydroxide dressings within the cleansed canals. If successfully arrested, the normal periodontal ligament will establish itself again over some period, and the endodontic seal can be completed. When there is extensive damage that is so bad that it has broken into the canal space from the root surface, additional repair is attempted by surgically exposing the defect, preparing a Class I cavity preparation, and filling the defect with a nondiscoloring material. The choice of material depends on the location of the problem; however, a resin-modified glass ionomer cement (Figures 19-64A to E) (ie, Geristore, DEN-MAT,
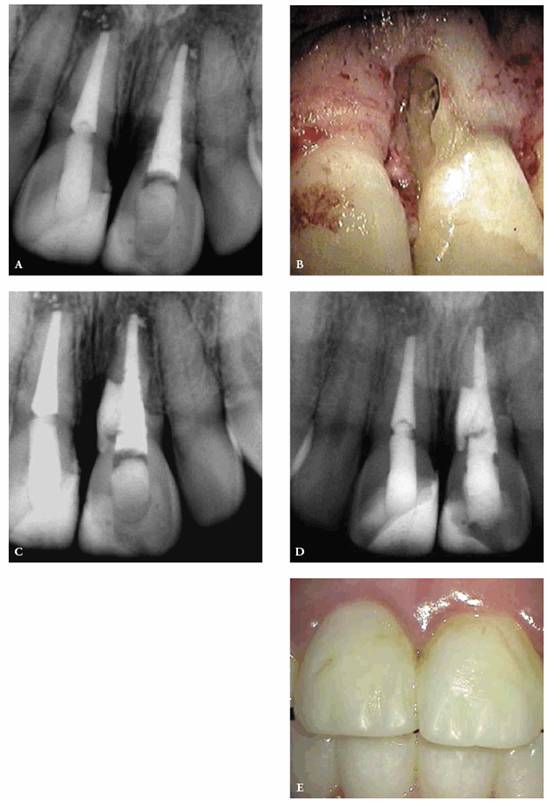
Figure 19-64A to E: Maxillary central incisor-surgical repair of resorptive defect following replantation. (A) Radiograph of a resorptive defect at cervical region following replantation, calcium hydroxide treatment, and root filling. Patient was 10 years old at this time. (B) Photograph showing the extent of the defect on the root. (C) Geristore (DEN-MAT) repair of the resorptive lacunae. (D) Check at 41/2 years discloses a return to the normal periradicular bone pattern. (E) Photograph of the resin-bonded repairs that will be replaced with laminates.
ENDODONTIC SURGERY
Although the technological advancements in endodontics have improved the rate of success, the demands of the populace to save teeth present degrees of difficulty that test the best of conventional therapy. In an effort to satisfy these demands, we are often called on to overcome anatomic, dentistogenic, or traumatic complications by intervening surgically. Sealing portals of exit surgically, for example, post perforations (Figures 19-65A and B), root resorption lesions (see Figures 19-64A to D), and inadequate root fillings where nonsurgical treatment is not practical (Figures 19-66A to C) constitute an extension of endodontic therapy and are alternatives to extraction.
Within the endodontic community, there is an emphasis on re-treating wherever possible and feasible rather than resorting to surgery as the first treatment option. The advent of sophisticated techniques, equipment, and materials allows for the nonsurgical retreatment of teeth that were heretofore candidates for extraction (Figures 19-67A to C).
Since endodontic surgery requires incising and elevating the soft tissue from bone, the obvious esthetic consequences can be recession and scarring. For these reasons, the choice and location of the surgical flap must be carefully evaluated before a scalpel ever touches tissue.5 There are several major flap designs that could be used, depending on existing restorations and anatomic factors.
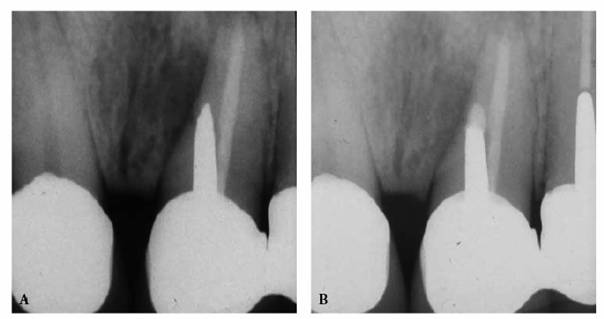
Figure 19-65A and B: Post perforation repair: (A) post perforation maxillary central incisor tooth and (B) 5 years after the surgical repair of the defect with IRM (DENTSPLY/Caulk).
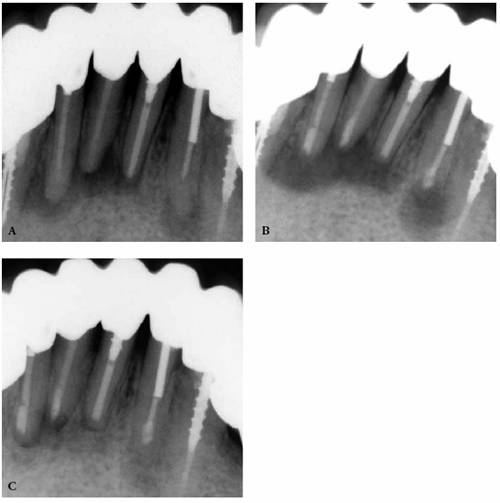
Figure 19-66A to C: Surgical re-treatment of mandibular anterior teeth: (A) preoperative radiograph, (B) mineral trioxide aggregate seals of the mandibular central and lateral incisors, and (C) 18-month check-up radiograph shows evidence of bone deposition.
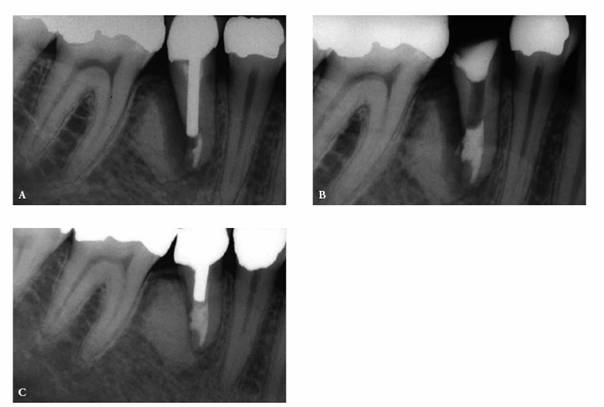
Figure 19-67A to C: Nonsurgical repair of a post perforation. (A) Preoperative radiograph of a mandibular premolar tooth. The position of the strip perforation on the distal surface obviates the possibility of surgical repair. (B) The crown, core build-up, and post were removed. The perforation was sealed with MTA. The tooth was restored with a cast post and a porcelain-fused-to-metal crown. (C) Six years later, the tooth is asymptomatic, and there is complete bone regeneration of the bone in the defect site.
TISSUE DISCOLORATION (TATTOO)
In the past, silver amalgam was the material of choice for retrofilling teeth when nonsurgical therapy could not be accomplished. The same material was indicated for the repair of perforations and resorptions. In a tissue environment, this material is notorious for its discoloring effect. Once the black tattoo occurs, corrective treatment requires removal of the cause, excising the tattoo, and grafting tissue across the defect. Such treatment can now be avoided by using either zinc oxide- and eugenol-based filling material (Super EBA, H.J. Bosworth, Skokie, IL, or IRM, DENTSPLY/Caulk), composite resin, glass ionomer cements (Geristore), or MTA because not only do they seal better than amalgam, they also do not cause the staining that is associated with the amalgam.
SUMMARY
Endodontic therapy may be the key to long-term maintenance of esthetic restorations. It is essential that the patient is aware of this fact from the outset. This way, there will be no misunderstanding about "fault" if pain should arise. Thus, a well-informed patient will continue to be a trusting patient who values these services throughout the life of the dental procedures.
REFERENCES
1. Abou-Rass M. The stressed pulp condition: an endodontic-restorative diagnostic concept. J Prosthet Dent 1982;48:264.
2. Andreasen JO, Andreasen FM. Essentials of traumatic injuries to teeth.
3. Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 4. Factors related to periodontal ligament healing. Endodont Dent Traumat 1995;11:76-89.
4. Arens DE, Chivian N. Endodontic contributions to esthetic dentistry.
5. Arens DE, Torabinejad M, Chivian N, Rubinstein R. Practical lessons in endodontic surgery. 3rd edn.
6. Barthel CR, Rosenkranz B, Lwuenberg A, Roulet JF. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endodont 2000;26:525-8.
7. Bohannan H, Abrams L. Intentional vital extirpation in periodontal prosthesis. J Prosthet Dent 1961;11: 781-9.
8. Dummer PMH, Hicks R, Huws D. Clinical signs and symptoms in pulpal disease. Int Endod J 1980;13: 27-35.
9. Ford TR, Torabinejad M, Abedi HR, et al. Using mineral trioxide aggregate as a pulp-capping material. J Am Dent Assoc 1996;127:1491-4.
10. Glockner K, Rumpler J, Ebeleseder K, Stadtler P. Intrapulpal temperature during preparation with the er: YAG laser compared to the conventional bur: an in vitro study. J Clin Laser Med Surg 1998;16:153-7.
11. Heithersay GS. Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg 1973;3:404.
12. Hunter FA. Saving pulps. A queer process. Dent Item Int 1883;5:352.
13. Ingram TA, Peters DD. Evaluation of the effects of carbon dioxide used as a pulpal test. Part 2: in vivo effect on canine enamel and pulpal tissues. J Endodont 1983;9:296-303.
14. Jimenez-Rubio A,
15. Lado EA, Stanley HR, Weissman MI. Cervical resorption in bleached teeth. Oral Surg 1983;55:78.
16. Langeland K. Prevention of pulpal damage. Dent Clin North Am 1972;16:709-32.
17. Madison S,
18. Madison S, Walton R. Cervical root resorption following bleaching of endodontically treated teeth. J Endodont 1990;16:570-4.
19. McMullen AF,
20. McMullen AF,
21. Michanowicz AE, Michanowicz JP. Endodontic access to the pulp chamber via porcelain jacket crowns. Oral Surg 1962;15(Suppl 2):S1483-8.
22. Pameijer CH, Stanley HR. The disastrous effects of the "total etch" technique in vital pulp capping in primates. Am J Dent 1998;11:S45-54.
23. Peters D, Lorton L, Mader C, et al. Evaluation of the effects of carbon dioxide used as a pulpal test. Part I: in vitro effect of human enamel. J Endodont 1983;9: 219-27.
24. Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endo J 1995;28:12-8.
25. Rivera EM, Vargas M, Ricks-Williamson L. Considerations for the aesthetic restoration of endodontically treated teeth following intracoronal bleaching. Pract Periodont Aesthet Dent 1997;9:117-28.
26. Spasser HF. A simple bleaching technique using sodium perborate. N Y State Dent J 1961;27:332-4.
27. Stanley HR. Human pulp response to restorative dental procedures.
28. Stanley HR, Swerdlow H. Reaction of the human pulp to cavity preparation: results produced by eight different operative techniques. J Am Dent Assoc 1959; 58:49.
29. Stokes AN, Tidmarsh BG. A comparison of diamond and tungsten carbide burs for preparing endodontic access cavities through crowns. J Endodont 1988; 14:11.
30. Teplitsky PE, Sutherland JK. Endodontic access of Cerestore crowns. J Endodont 1985;11:12.
31. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endodont 1999;25:3.
32. Trope M, Chivian N, Sigurdsson A. Trauma. In: Pathways of the pulp. 8th edn. St. Louis: Mosby, 2001: 603-49.